HPV and Male Fertility: Understanding the Impact
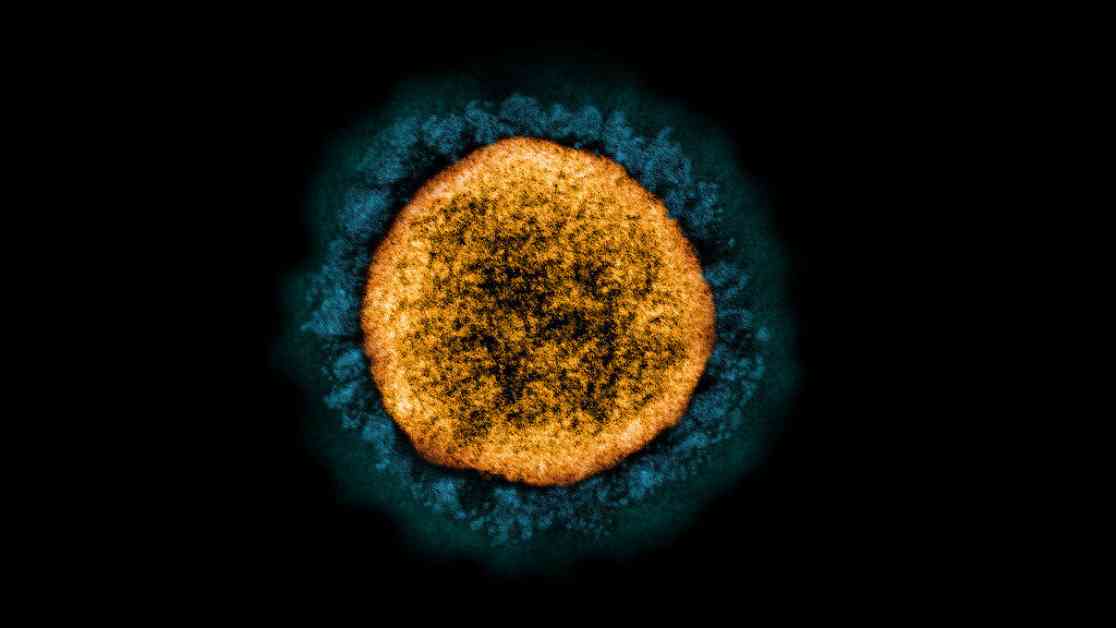
Human papillomavirus (HPV) has long been recognized as the most common sexually transmitted infection globally, with significant implications for reproductive health. While much of the research on HPV’s effects on fertility has traditionally focused on its impact on women, recent studies have shed light on its potential consequences for male fertility as well. A new study conducted by researchers in Argentina has highlighted the prevalence of high-risk strains of HPV in men and their potential impact on sperm quality.
The Study on HPV and Male Fertility
The study, published in Frontiers in Cellular and Infection Microbiology, examined the presence of high-risk HPV strains in a cohort of 205 men seeking fertility assessment or treatment for urinary tract issues. The researchers found that high-risk HPV strains, known for their association with cancer, were more prevalent than low-risk strains among the participants. Interestingly, the study also revealed that high-risk HPV appeared to suppress key components of the immune system in the male genital tract, potentially compromising the body’s ability to clear the infection.
According to Virginia Rivero, the senior author of the study and a professor of immunology at the National University of Córdoba in Argentina, individuals infected with HPV may not exhibit any symptoms but still carry the virus in their genital tract. This stealthy nature of HPV infection in men underscores the importance of understanding its potential impact on fertility.
The Impact on Sperm Quality
One of the key findings of the study was the correlation between high-risk HPV infection and compromised sperm quality. Men with high-risk HPV strains in their semen were found to have lower levels of certain immune cells, suggesting that the virus had impaired the body’s ability to combat the infection. This immune suppression not only increased the risk of persistent HPV infection but also raised the likelihood of other infections that could further jeopardize male fertility.
Furthermore, the study revealed evidence of oxidative stress-induced damage to sperm in men infected with high-risk HPV strains. This damage could explain the higher proportion of dead sperm observed in these individuals compared to those without the virus. Dr. Eugenio Ventimiglia, an oncologist specializing in urology, emphasized the importance of these findings in elucidating the biological mechanisms linking HPV to male reproductive health issues.
Implications for Male Infertility
The study’s results have significant implications for male infertility, with researchers noting that 21% of infertile men tested positive for HPV in their semen, compared to only 8% in the general male population. Even after accounting for female infertility factors, men with HPV in their semen were found to have a three-fold greater likelihood of being infertile than those without the virus. This underscores the need for greater awareness of HPV’s impact on male fertility and the importance of targeted interventions.
HPV and Cancer Risk
While HPV is commonly associated with cervical cancer, the virus can also cause other malignancies, including vulval, anal, throat, vaginal, and penile cancers. In the United States alone, HPV is responsible for tens of thousands of cancer diagnoses each year, highlighting the urgent need for preventive measures. Vaccination against HPV has been available since 2006, with the current vaccine targeting nine of the most high-risk HPV strains, including those that cause genital warts.
The Importance of HPV Vaccination
The Centers for Disease Control and Prevention (CDC) recommend routine HPV vaccination for all boys and girls starting at age 11 or 12, with the option to receive the vaccine as early as age 9. Adolescents and young adults up to age 26 who were not previously vaccinated are also encouraged to get the HPV vaccine. Recent data from the CDC revealed a slight decrease in HPV vaccination rates among adolescents born in 2008 compared to those born in 2007, attributed in part to disruptions caused by the COVID-19 pandemic.
Despite the proven efficacy and safety of the HPV vaccine, there remains a need to increase vaccination rates among boys and men to protect against HPV-related cancers and potentially safeguard male fertility. Dr. Marie-Hélène Mayrand, an epidemiologist specializing in obstetrics and gynecology, emphasized the temporary nature of HPV infection and its limited impact on fertility, providing reassurance to individuals concerned about the virus’s effects.
The Role of HPV Vaccination in Male Fertility
While the HPV vaccine has demonstrated significant benefits in reducing cancer risk, its potential impact on male fertility remains uncertain. Rivero highlighted the need for further research to explore the broader implications of HPV vaccination on male reproductive health. A larger study focusing on simultaneous HPV and other sexually transmitted infections (STIs) could provide valuable insights into how these infections collectively influence male fertility.
Rivero’s lab plans to investigate how HPV and other STIs interact to affect male fertility, shedding light on the complex interplay between infectious agents and reproductive health. By identifying specific strains of HPV and their impact on fertility, men struggling with infertility can receive targeted interventions to address underlying causes and improve their chances of conception.
Conclusion
HPV’s association with male fertility represents a growing area of research that warrants attention and further exploration. The findings from the Argentine study underscore the need for comprehensive screening and vaccination programs to protect against HPV-related complications, including infertility. By raising awareness of the potential impact of high-risk HPV strains on male fertility and promoting preventive measures, we can empower individuals to take proactive steps towards safeguarding their reproductive health.