Georgina Peacock shared a poignant memory of a night during her pediatric medical training when she admitted 20 babies struggling to breathe due to Respiratory Syncytial Virus (RSV). Since then, efforts have been relentless to overcome obstacles hindering the delivery of two new tools that promise to revolutionize the approach to RSV and reduce hospitalization rates. One tool is a Pfizer vaccine administered late in pregnancy to provide antibodies to the fetus, while the other is an antibody injection called Beyfortus (nirsevimab) given to infants before their first RSV season, especially high-risk babies.
Peacock emphasized the potential life-changing impact of immunizing children against RSV through these tools, as it could significantly reduce hospital admissions. This year’s rollout of the new medical tools is expected to be smoother than the previous year, with improvements in supply and distribution. However, challenges remain in ensuring timely delivery to those in need, including birthing hospitals, pediatricians, obstetricians, and pharmacies.
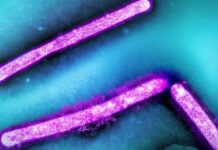
RSV, a common virus causing cold-like symptoms, particularly affects older adults and infants, leading to severe illness. It is the primary cause of infant hospitalizations in the U.S., with seasonal peaks in activity during fall and winter. The recent approval of vaccines and antibody injections for RSV has brought hope to the pediatric care community, although the cost of these products is a concern.
The Pfizer maternal vaccine and Beyfortus injections are priced high, posing financial challenges for healthcare providers and hospitals. While efforts are being made to facilitate access to these tools, affordability remains a significant issue for uninsured individuals. Strategies such as the Vaccines for Children program help cover costs for eligible babies, but enrollment of birthing hospitals in the program is crucial for broader access.
Despite the financial hurdles, the effectiveness of Beyfortus in preventing RSV hospitalization has been promising, with a reported 90% effectiveness rate in a recent CDC study. The gradual integration of these tools into healthcare delivery systems is expected to take time, with ongoing efforts to improve distribution and increase coverage among eligible infants.
While the path to widespread protection against RSV may be challenging, healthcare professionals remain hopeful that the societal benefits of these new tools will soon become evident. With a concerted focus on addressing distribution challenges and expanding access, the goal of reducing RSV-related hospitalizations in infants is within reach.