Addressing the Underutilization of Effective Menopause Symptom Treatment
At the annual Menopause Society meeting this fall, researchers revealed groundbreaking evidence supporting the benefits of hormone therapy for menopausal women. This therapy not only improves heart health but also reduces insulin resistance and other cardiovascular biomarkers. Moreover, hormone therapy has proven effective in alleviating common menopausal symptoms such as hot flashes, sleep disturbances, vaginal dryness, and pain during sex.
Why the Decline?
Despite the overwhelming evidence supporting hormone therapy, its utilization among menopausal women has drastically declined over the past few decades. In 1999, nearly 27% of menopausal women in the U.S. used estrogen, but by 2020, that number plummeted to less than 5%.
Experts attribute this decline to misconceptions about the risks associated with hormone therapy and the prevailing cultural taboo surrounding discussions about menopause. The combination of these factors has created a perfect storm leading to the under-treatment of menopausal women.
Understanding the Risks
The catalyst for the decline in hormone therapy usage was the 2002 Women’s Health Initiative study, which suggested an increased risk of heart disease and breast cancer associated with hormone therapy. This study, focusing on older postmenopausal women not experiencing symptoms like hot flashes, led to a significant decrease in hormone therapy uptake.
However, subsequent research has indicated that the risk of adverse events from hormone therapy is low for menopausal women, particularly those under the age of 60 seeking relief from their symptoms. While assessing risks for postmenopausal women is more complex, recent studies have provided valuable insights into the benefits and potential risks associated with hormone therapy.
Personalizing Treatment
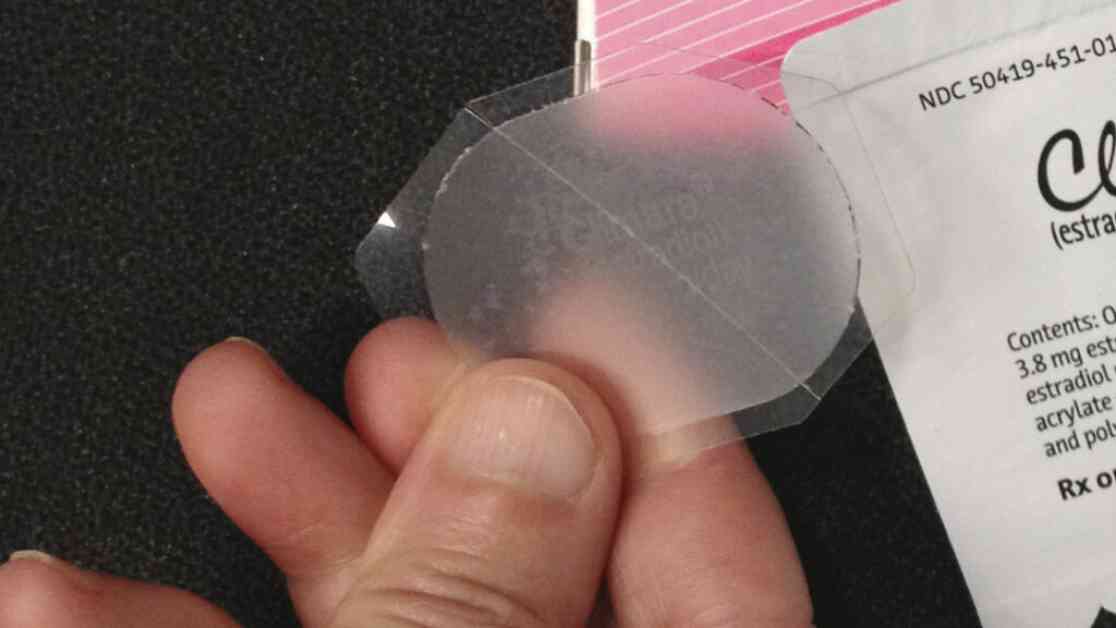
When considering hormone therapy for menopause, individuals must weigh their symptoms and personal philosophies on aging. Some may seek relief from classic symptoms like hot flashes, while others may prioritize aesthetic concerns or osteoporosis prevention. Conversely, some individuals may opt out of hormone therapy due to family history of certain conditions or personal aversion to medication.
Providers such as OB-GYN Robin Noble, a certified menopause practitioner, emphasize the importance of informed decision-making and individualized treatment plans. With a growing need for better understanding of menopause treatment among healthcare providers, efforts are underway to educate both physicians and patients on the safety and effectiveness of hormone therapy.
In conclusion, the key takeaway is that there are various options available for menopausal women seeking relief from symptoms. By making informed decisions based on individual needs and preferences, women can explore the potential benefits of hormone therapy tailored to their specific health status and risk factors.