Understanding Metastatic Cancer: Causes, Symptoms, and Treatment Options
A cancer diagnosis can be a frightening experience for anyone. While some cancers can be cured if caught early, others can be much more challenging to treat, especially once they have spread to other parts of the body. Cancer cells are notorious for their ability to grow and spread, making treatment difficult and sometimes ineffective.
Metastatic cancer, also known as metastasis, occurs when cancer cells break away from their original site and travel to other organs in the body. This migration can disrupt the normal function of these organs, leading to life-threatening complications. In fact, it is estimated that about 90% of cancer-related deaths are caused by metastatic cancer rather than the primary tumor.
Researchers have been working tirelessly to better understand how metastasis occurs in order to develop new and more effective ways to prevent or treat it. Thanks to advancements in medical technology, some individuals with metastatic cancer can now live for many years if the disease is well-controlled.
Adapting to New Locations
Cancer cells have the ability to spread to almost any part of the body, with the liver, lungs, and bones being the most common sites for metastasis. Different types of cancer have a tendency to spread to specific locations; for example, pancreatic and colon cancer often spread to the liver, while breast cancer and melanoma can spread to the brain.
It’s important to note that metastatic cancer is considered to be the same type of cancer as the original tumor, even though it has migrated to a new location. Dr. Rosandra Kaplan, a physician and cancer researcher at the National Institutes of Health (NIH), explains, “Breast cancer that spreads to the bone is still considered to be breast cancer, not bone cancer. It’s usually the original cancer that has found a way to escape and grow in a new location.”
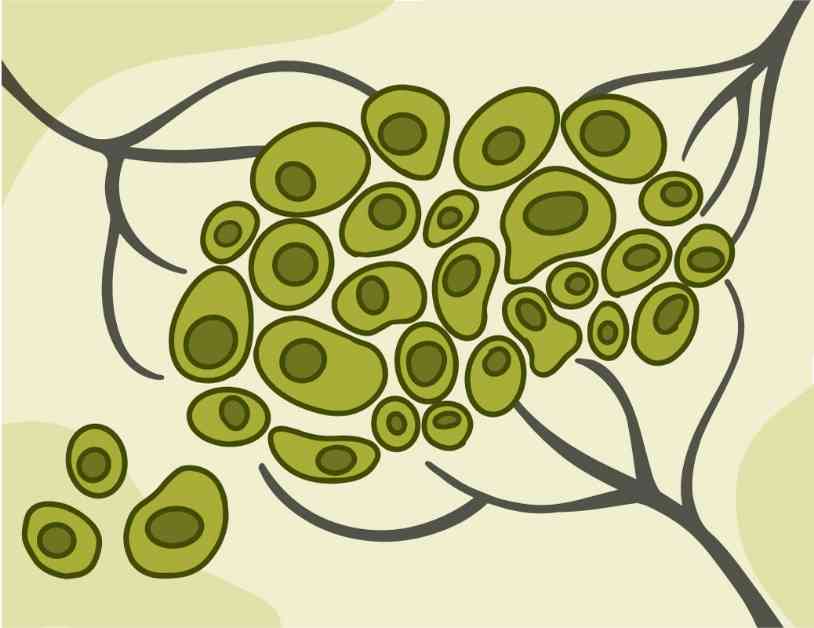
Researchers have been investigating the mechanisms through which cancer cells spread to new sites in the body. Once these cells break away from the primary tumor, they can travel through blood vessels to other parts of the body. While the immune system typically destroys these escaping cells, some may survive and establish themselves in a new location. These cells can then form a cluster that stimulates the growth of new blood vessels, providing the metastatic tumor with a blood supply to thrive.
Cancer cells undergo significant changes in order to survive in a new environment, although they retain some characteristics of the original tumor cells. Dr. Karuna Ganesh, a physician scientist at Memorial Sloan Kettering Cancer Center, emphasizes that metastatic cancers become increasingly different from the primary tumors they originated from, making them more challenging to treat.
Revving Up Defenses
In recent years, researchers have made significant strides in utilizing the body’s own immune system to combat cancer through a treatment known as immunotherapy. One type of immunotherapy, called immune checkpoint inhibitors, has shown promise in extending the lives of patients with metastatic cancer.
Dr. Christine Nadeau, an expert on metastasis at NIH, explains, “Tumor cells have the ability to evade the immune system by displaying proteins that signal ‘Do not attack me.’ Immune checkpoint inhibitor drugs block these signals, allowing the immune cells to recognize and destroy the cancer cells.”
While immune checkpoint inhibitors have been effective in treating metastatic melanoma and certain types of kidney, lung, head, and neck cancers, they are not effective for everyone and can have harsh side effects. Researchers are now developing artificial intelligence tools to help identify patients who are most likely to benefit from these drugs, ensuring that those who will not benefit can receive alternative treatments.
Another form of immunotherapy, known as cell-based therapy, involves using a patient’s own immune cells as a treatment against cancer. Dr. Kaplan explains, “Cell therapies involve extracting the patient’s immune cells, modifying them to enhance their ability to target cancer cells, and then reintroducing them into the patient’s bloodstream.”
One particular type of cell therapy, called CAR T-cell therapy, has been used to treat blood cancers like leukemia for years. In early 2024, the U.S. Food and Drug Administration approved the first cell-based therapy for solid tumors, specifically for metastatic melanoma. Clinical trials are also underway to explore the use of cell therapy in treating metastatic colon and breast cancers.
Coping With Metastatic Cancer
Receiving a diagnosis of metastatic cancer can be overwhelming for patients and their families. However, there is reason to remain hopeful as treatment options continue to evolve and improve. The primary goal of treating metastatic cancer is usually to control its growth and extend the patient’s lifespan, while also focusing on symptom management and quality of life through palliative care.
Dr. Nadeau suggests that joining advocacy or support groups specific to a patient’s type of cancer can provide valuable support and resources. These groups often consist of individuals who have undergone similar treatments and can offer insights and guidance on navigating the challenges of living with metastatic cancer.
In conclusion, while metastatic cancer presents significant challenges in treatment and prognosis, ongoing research and advancements in therapies like immunotherapy offer hope for improved outcomes and quality of life for patients. By continuing to explore new treatment options and approaches, we move closer to better understanding and effectively managing metastatic cancer.