Decades of NIH Research Reveals Insights on Rare Bone, Skin, and Endocrine Disorder
Patients with fibrous dysplasia/McCune-Albright Syndrome often face challenges such as easily breaking bones, early puberty, and potential vision and hearing loss. For years, doctors have been trying to understand why these symptoms occur and how to effectively treat them.
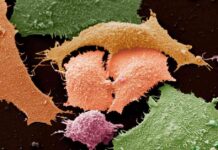
Fibrous dysplasia/McCune-Albright Syndrome, also known as FD/MAS, is a genetic disease that affects both bones and the skin and endocrine system. Although there is no cure for this condition, advancements in research have led to more effective treatments and management strategies for patients.
FD/MAS is a genetic disease that develops during fetal development, with early signs including large birthmarks and premature puberty. The complications of FD/MAS can range from mild to severe, impacting the quality of life of those affected. Treatments for FD/MAS may include surgery, hormone therapy, or medical device implants to manage symptoms and improve quality of life.
Research by Drs. Allen Spiegel, Janice Lee, Pamela Robey, Michael Collins, and Mara Riminucci has been instrumental in advancing our understanding of FD/MAS and developing treatment options for patients. Dr. Spiegel’s research in 1991 identified a specific protein mutation responsible for the skin and hormonal effects of FD/MAS, while Dr. Robey’s work revealed how the same mutation affects bone lesions.
A natural history study initiated in 1998 has provided valuable insights into how FD/MAS progresses over a person’s lifespan. By examining patients of all ages and tracking their symptoms, bone scans, and responses to treatments, researchers have been able to create more personalized treatment plans for patients. Clinical decision-making guidelines published in 2015 have further aided clinicians in developing appropriate treatment plans based on individual symptoms.
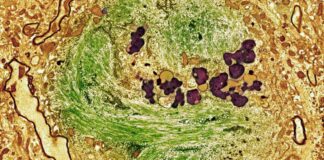
While there are medications available to treat hormonal symptoms of FD/MAS, such as hyperthyroidism, there is currently no way to stop the growth of bone lesions. Ongoing research is exploring the use of drugs like denosumab to prevent the formation of bone lesions in children with FD/MAS. Additionally, studies on burosumab are being conducted to improve blood phosphate levels in patients with FD/MAS, as maintaining adequate phosphate levels is crucial for bone health.
Despite significant progress in understanding and treating FD/MAS, there is still much to learn about this complex genetic disorder. Continued research efforts supported by the NIH aim to further enhance our knowledge of FD/MAS and develop innovative treatment strategies to improve the lives of patients affected by this rare condition.