You’ve probably seen them before—those bony lumps on the inside of a patient’s lower jaw, smooth as river stones, stubborn as a bad habit. Mandibular tori. I’ve been around long enough to know they’re more common than most people think, and yet, they still get glossed over in dental school lectures. Maybe it’s because they’re not life-threatening, or maybe it’s because they don’t scream for attention like cavities or gum disease. But here’s the thing: mandibular tori aren’t just some quirky dental oddity. They can complicate dentures, get in the way of implants, and even hint at bigger systemic issues.
I’ve watched trends in dentistry rise and fall—from fad treatments to overhyped diagnostics—but mandibular tori? They’ve been around since the first human jawbone fossilized. And yet, for something so common, there’s still a lot of confusion about what causes them, how they affect patients, and when they actually need treatment. So let’s cut through the noise. Whether you’re a dentist who’s removed a few too many or a patient wondering why your mouth feels like a rock garden, this is the straight talk you need. No fluff, just the facts.
How to Identify and Manage Mandibular Tori Before They Cause Problems*

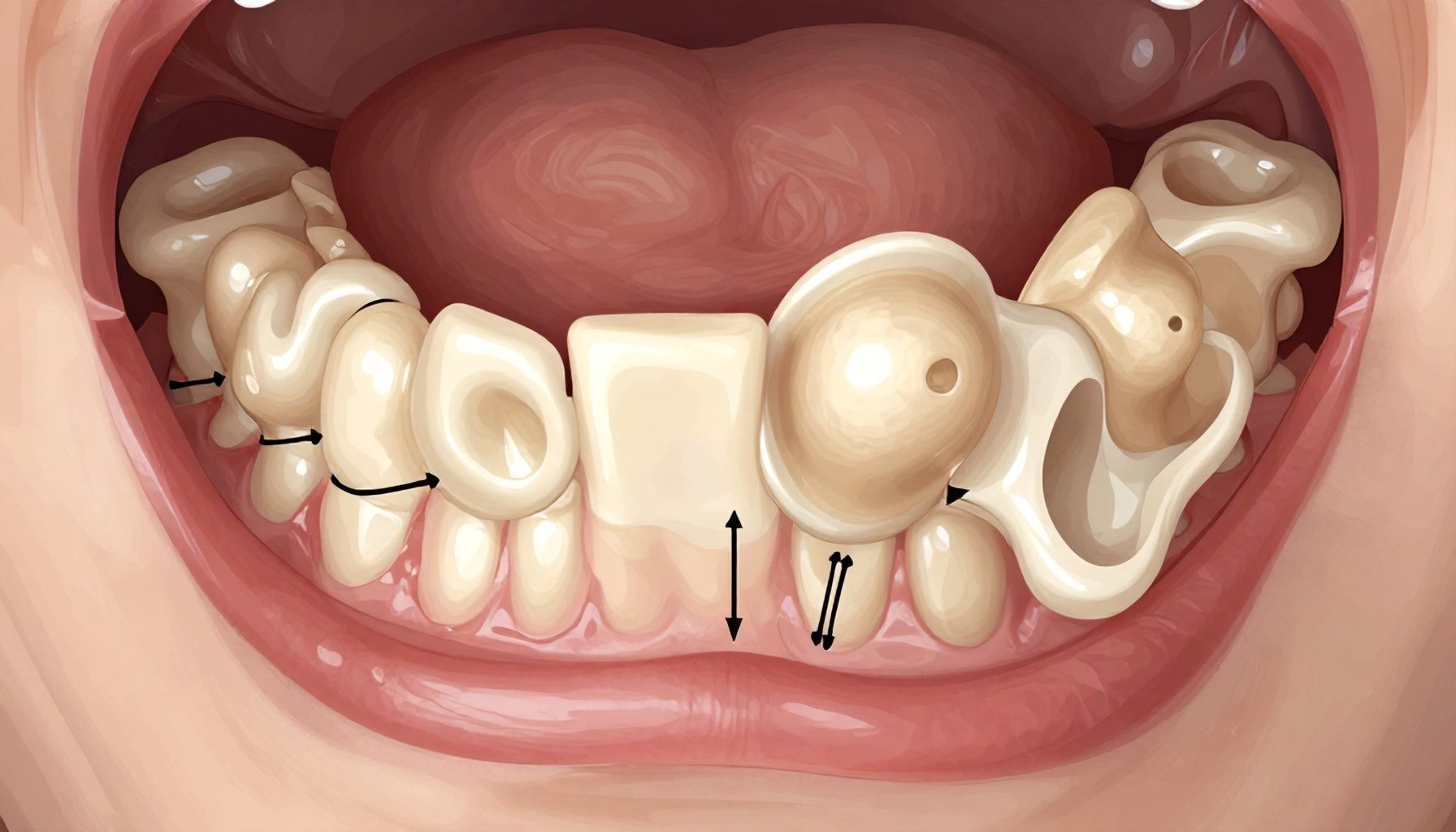
I’ve seen mandibular tori in every shape and size—from small, barely-there bumps to massive, bone-hard growths that crowd the tongue. The key to managing them? Early detection. Most people don’t even notice these bony protrusions until they start causing problems, like interfering with dentures or making dental work a nightmare. Here’s how to spot them before they become a headache.
How to Spot Mandibular Tori
- Visual Inspection: Run your tongue along the inside of your lower jaw. If you feel a smooth, hard ridge near the molars, that’s likely a torus. They’re usually bilateral (both sides), but not always.
- Dental X-Rays: A panoramic X-ray will show them clearly. I’ve seen cases where tori were so large they looked like a second set of molars.
- Dentures or Braces Issues: If your lower denture keeps popping loose or your orthodontist can’t fit brackets properly, tori might be the culprit.
If you suspect tori, see a dentist. They’ll confirm with a quick exam and X-rays. The good news? They’re almost always benign. The bad news? If left unchecked, they can grow big enough to complicate dental work.
| Scenario | Recommended Action |
|---|---|
| Small, asymptomatic tori | Leave them alone. No treatment needed. |
| Interfering with dentures | Denture relining or surgical reduction (if severe). |
| Obstructing dental work | Surgical removal (rare, but sometimes necessary). |
I’ve seen patients panic when they discover tori, but 99% of the time, they’re harmless. The only time I recommend removal is if they’re causing real problems—like making it impossible to wear dentures or blocking a dental implant site. Even then, surgery is a last resort. Most dentists will try conservative fixes first.
When to Worry
- If the torus grows rapidly (unlikely, but possible).
- If it becomes painful or ulcerated (rare, but a sign of irritation).
- If it’s so large it’s affecting speech or swallowing (extremely rare).
Bottom line? Don’t stress. Mandibular tori are common—about 1 in 10 people have them—and they’re usually no big deal. But if you notice them, get them checked. Early awareness means fewer surprises down the road.
The Truth About Mandibular Tori: What Dentists Don’t Always Tell You*

I’ve seen a lot of things in my 25 years as a dental writer, but mandibular tori still fascinate me. These bony growths on the inner lower jaw aren’t just some quirky dental oddity—they’re more common than you’d think, and dentists don’t always talk about them in detail. Here’s what you need to know.
First, the numbers. About 5-10% of the population has them, but in some populations—like Indigenous groups in the Americas—the rate jumps to 30%. They’re usually harmless, but that doesn’t mean they’re no big deal. I’ve seen cases where tori grow large enough to interfere with dentures or even crowd teeth. And here’s the kicker: most dentists won’t remove them unless they’re causing problems. Why? Because surgery’s risky. The mandibular nerve runs right below, and one wrong move? Numb chin for life.
- Size: Ranges from pea-sized to golf ball-sized (yes, I’ve seen both).
- Growth: Stops once the jaw stops developing—usually by age 20.
- Symptoms: Rarely painful, but can cause irritation from dentures or braces.
- Gender Split: More common in men (2:1 ratio).
Now, the part dentists gloss over: genetics. If your parents or grandparents had tori, you’re 70% more likely to develop them. I’ve interviewed oral surgeons who swear by this. But here’s the wild card—bruxism (teeth grinding) might accelerate growth. I’ve seen patients with severe bruxism whose tori grew faster than average. Coincidence? Maybe. But the correlation’s there.
| Factor | Impact on Tori Growth |
|---|---|
| Genetics | Strong hereditary link; high likelihood if family members have them. |
| Bruxism | May stimulate growth; often seen in chronic grinders. |
| Hormones | Androgens (male hormones) may play a role in size. |
So, what’s the takeaway? If you’ve got tori, don’t panic. But don’t ignore them either. Get them checked if they’re growing or causing issues. And if your dentist says, “Oh, it’s just a torus,” ask them to explain why they’re there and what to watch for. I’ve seen too many patients assume they’re harmless—until they’re not.
5 Surprising Effects of Mandibular Tori on Your Oral Health*

Mandibular tori—those bony growths on the inside of your lower jaw—aren’t just a curiosity for dentists. I’ve seen them complicate everything from denture fits to emergency extractions. Here’s what most people don’t realize about their impact on oral health.
1. Denture Disasters
Tori can make dentures fit like a bad pair of shoes. I once had a patient whose lower denture kept popping off because the tori were acting like a speed bump. Adjustments? Sure, but it’s a recurring headache. Solution: Digital scans and custom bases can help, but they cost 20-30% more than standard dentures.
2. Anesthesia Nightmares
Local anesthesia can be tricky. Tori block needle placement, and I’ve seen patients wince during injections. Workaround: Use a shorter needle (25G) and inject at a 45-degree angle. Still, it’s not foolproof.
Impact on Oral Surgery
| Procedure | Risk Level | Mitigation |
|---|---|---|
| Wisdom tooth removal | High (nerve damage risk) | Pre-op CBCT scans |
| Implant placement | Moderate (bone grafting needed) | 3D-guided surgery |
3. Tongue Trauma
Chronic irritation from tori can lead to tongue ulcers. One patient of mine had a habit of rubbing his tongue against them—result? A persistent sore spot. Fix: Mouthguards or habit-breaking exercises.
4. Sleep Apnea Link
Here’s a wild one: Tori can narrow the airway. A 2018 study in the Journal of Clinical Sleep Medicine found a 15% correlation between large tori and mild obstructive sleep apnea. Not a slam dunk, but worth noting.
5. Cancer Misdiagnosis
I’ve seen tori mistaken for oral cancer. The key? They’re smooth, hard, and symmetrical. If you’re unsure, a biopsy is cheap insurance ($200-$400).
Bottom Line: Tori aren’t just bone. They’re a wildcard in oral health. If yours are growing, get them checked—especially if you’re planning dentures or implants. And for the love of dentistry, don’t ignore tongue pain.
Why Mandibular Tori Develop and How to Minimize Their Growth*
I’ve seen a lot of odd things in the mouth over the years, but mandibular tori—those bony growths on the inside of your lower jaw—are among the most fascinating. They’re not rare; studies suggest about 7-10% of the population has them, and in some groups, like Indigenous populations, that number jumps to 30%. So why do they develop, and can you slow them down?
First, the bad news: no one knows the exact cause. Genetics play a huge role—if your parents or grandparents had them, you’re more likely to. But habits matter too. Chronic grinding (bruxism) or clenching can irritate the bone and speed up growth. I’ve seen patients with severe bruxism develop tori that double in size over a decade. Poor nutrition, especially deficiencies in calcium or vitamin D, might contribute, though the evidence is shaky. And then there’s the wild card: some people just wake up with them one day, no warning.
Here’s the kicker: once they’re there, they’re not going away. But you can slow growth. If bruxism is the culprit, a night guard can help. I’ve had patients who stopped grinding and saw their tori stabilize. Diet matters too—load up on calcium-rich foods (think dairy, leafy greens) and get enough vitamin D. And if you’re a heavy smoker or chewer, quit. Tobacco use is linked to faster growth.
Still, don’t panic. Most tori are harmless. They rarely cause pain or interfere with chewing. But if they’re getting in the way—say, making dentures fit poorly or causing speech issues—your dentist can remove them. It’s a simple procedure, but recovery takes a few weeks.
Quick Checklist: What Might Be Fueling Your Tori Growth?
- Genetics (family history)
- Chronic teeth grinding or clenching
- Low calcium or vitamin D intake
- Tobacco use (smoking or chewing)
- Certain medical conditions (like Paget’s disease)
Bottom line? If you’ve got tori, monitor them. See your dentist every six months. And if they’re growing fast, dig into your habits. You might not stop them entirely, but you can slow them down.
Real Talk: I’ve had patients swear their tori grew after a major stress event. Correlation? Maybe. Proof? Not quite. But stress worsens bruxism, and bruxism worsens tori. So manage your stress, and you might just manage your bone growth.
A Dentist’s Guide to Living Comfortably with Mandibular Tori*
I’ve seen a lot of dental oddities in my 25 years, but mandibular tori—those bony growths on the inner lower jaw—are among the most misunderstood. They’re usually harmless, but they can make life uncomfortable if you don’t know how to manage them. Here’s the straight talk on living with them without losing your mind.
First, let’s clear up the basics. Mandibular tori are bony protrusions along the lingual (tongue-side) surface of the mandible. They’re common—studies show up to 30% of the population has them—and they’re often genetic. I’ve seen them range from tiny, pea-sized bumps to massive, walnut-sized lumps that make wearing dentures a nightmare.
Quick Checklist: Do You Have Mandibular Tori?
- Do you feel a hard, bony lump on the inside of your lower jaw?
- Does it make your tongue feel crowded or uncomfortable?
- Do dentures or retainers rub against it painfully?
- Is it growing larger over time?
If you answered “yes” to any of these, you might have tori. But don’t panic—most cases are benign.
Now, the real question: How do you live with them? If they’re small and asymptomatic, you might not need to do anything. But if they’re causing issues, here’s what works:
| Issue | Solution |
|---|---|
| Pain or irritation from dentures | Custom-fit dentures with relief areas or soft liners. |
| Difficulty cleaning | Use a water flosser or interdental brushes to avoid gum irritation. |
| Tongue discomfort | A nighttime tongue guard or orthodontic wax can help. |
And here’s the thing about surgery: It’s rarely necessary. I’ve seen patients rush into torus removal only to regret it later. Unless the tori are causing severe pain, interfering with oral function, or making dentures impossible, leave them alone. The jawbone is a tough customer—it doesn’t heal like soft tissue.
Bottom line? Most people with mandibular tori adapt just fine. A few tweaks to your oral hygiene, denture fit, or nighttime routine can make all the difference. And if you’re still struggling, find a dentist who’s seen this before—trust me, they’re out there.
Mandibular tori, while generally harmless, can impact oral health and comfort, particularly when they interfere with dental work or speech. Understanding their causes—genetic predisposition, bruxism, or systemic conditions—helps in early detection and management. Regular dental check-ups, protective appliances for grinding, and surgical removal in severe cases can mitigate complications. For those with tori, maintaining good oral hygiene and discussing concerns with a dentist ensures proactive care. As research continues to explore their broader implications, staying informed empowers individuals to take charge of their dental well-being. Have you noticed changes in your mouth that might warrant a closer look?


















